Introduction
Cardiovascular diseases (CVD) are the world's leading cause of death, claiming an estimated 18.6 million lives annually. In the United States alone, CVD accounts for about one-third of all deaths. However, there's reason for optimism: according to the World Heart Federation's 2023 World Heart Report, up to 80% of premature heart attacks and strokes are preventable.
The insidious nature of CVD lies in its silent progression. Damage accumulates over time without obvious external signs, often manifesting only when significant harm has already occurred. This underscores the critical importance of understanding the underlying processes, particularly atherosclerosis—a primary driver of fatal cardiovascular events characterized by plaque buildup in the arteries.
While the average American diet and lifestyle contribute to CVD risk, there's substantial opportunity for prevention rather than just treatment. Understanding the cardiovascular system, its potential breakdowns, and implementing monitoring and prevention strategies can significantly reduce your risk of premature death or disability.
This article will explore the cardiovascular system, its vulnerabilities, and effective strategies for risk management. Cardiovascular health represents one of the highest-return investments you can make in your overall well-being. Like financial investments, the earlier you start, the better—but the second-best time to begin is now. By focusing on this crucial aspect of health, you can potentially add years to your life and improve its quality.
How Your Heart and Cardiovascular System Work
To understand atherosclerosis, we first need to grasp the basics of how your cardiovascular system functions. Think of your cardiovascular system as your body's highway network, with your heart as the central pump station. Understanding this system is crucial because atherosclerosis disrupts this finely tuned process, potentially leading to severe health consequences.
- The Heart: This fist-sized powerhouse is essentially a muscular pump. It has four chambers—two atria (upper chambers) and two ventricles (lower chambers)—that work together to circulate blood throughout your body.
- Blood Vessels: These are the roads of your cardiovascular highway:
- Arteries carry oxygenated blood away from the heart to the body's tissues.
- Veins return deoxygenated blood back to the heart.
- Capillaries are tiny blood vessels that connect arteries and veins, allowing for the exchange of oxygen, nutrients, and waste products with body tissues.
- The Circulatory Process:
- The right side of the heart pumps deoxygenated blood to the lungs, where it picks up oxygen and releases carbon dioxide.
- The left side of the heart then pumps this oxygen-rich blood to the rest of the body.
- As blood circulates, it delivers oxygen and nutrients to cells and collects waste products.
- Blood Composition: Blood isn't just a red liquid. It's a complex mixture that includes:
- Red blood cells (carrying oxygen)
- White blood cells (part of the immune system)
- Platelets (for blood clotting)
- Plasma (the liquid component, which carries nutrients, hormones, and proteins)
What is Atherosclerosis?
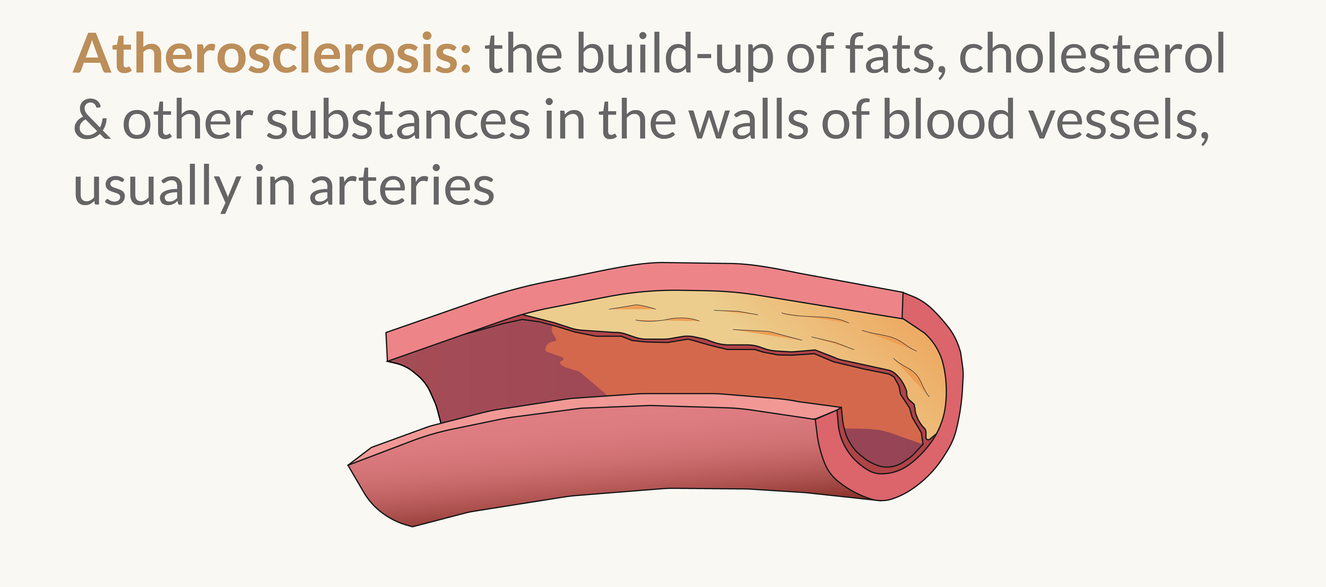
Atherosclerosis, the underlying cause of many cardiovascular diseases, is a complex process that affects the arteries. To understand it, imagine your arteries as smooth, flexible highways that transport blood throughout your body. Now picture these same highways slowly narrowing, becoming rigid and rough, with debris building up along the sides. This is atherosclerosis in action.
The Atherosclerotic Process
- Endothelial Dysfunction: The inner lining of arteries (the endothelium) becomes damaged due to factors like high blood pressure, smoking, or elevated blood sugar.
- Lipoprotein Entry: Damaged endothelium allows cholesterol-carrying particles, mainly LDL (low-density lipoprotein), to enter the artery wall.
- Inflammation: The presence of LDL triggers an inflammatory response. White blood cells (monocytes) enter the artery wall and transform into macrophages.
- Foam Cell Formation: Macrophages engulf oxidized LDL, becoming lipid-laden "foam cells."
- Plaque Development: Over time, this creates a buildup of cells, cholesterol, and debris – arterial plaque. The plaque can grow, narrowing the artery.
- Potential Rupture: In advanced stages, plaques can rupture, potentially causing a blood clot that blocks blood flow entirely.
Understanding this process is crucial for recognizing why atherosclerosis is so dangerous and why early prevention is key. In the following sections, we'll explore specific risk factors for atherosclerosis and discuss strategies for monitoring and managing your cardiovascular health to prevent its progression.
Hypertension
Hypertension, or high blood pressure, is often called "the silent killer" because it typically has no symptoms but can lead to severe health problems, including atherosclerosis. Let's break down what blood pressure is and how it relates to atherosclerosis:
- What is Blood Pressure?:
- Blood pressure is the force of blood pushing against the walls of your arteries as your heart pumps blood.
- It's measured in millimeters of mercury (mmHg) and recorded as two numbers: systolic pressure (when the heart beats) over diastolic pressure (when the heart is at rest).
- Normal blood pressure is generally considered to be below 120/80 mmHg.
- Hypertension and Endothelial Damage:
- High blood pressure can damage the endothelium (the inner lining of blood vessels).
- This damage makes it easier for LDL cholesterol to penetrate the artery walls, initiating the atherosclerotic process.
- Inflammation and Hypertension:
- Hypertension can trigger an inflammatory response in the blood vessels.
- This inflammation further damages the endothelium and accelerates atherosclerosis.
- Mechanical Stress:
- High blood pressure puts extra mechanical stress on the artery walls.
- Over time, this can lead to thickening and stiffening of the arteries, a condition known as arteriosclerosis.
- Vicious Cycle:
- As atherosclerosis progresses, arteries become narrower and less flexible.
- This can further increase blood pressure, creating a vicious cycle.
Managing blood pressure is crucial in preventing and managing atherosclerosis. Regular monitoring, lifestyle changes, and medication (if prescribed by a healthcare provider) can help keep blood pressure in check and reduce the risk of atherosclerosis and its complications.
Understanding Cholesterol and Lipoproteins
Cholesterol
- A waxy substance needed for various bodily functions, including building cell membranes and producing hormones.
- Despite its bad reputation, cholesterol is essential for life. The problem arises when there's too much of it in the bloodstream.
Lipoproteins
Particles that transport cholesterol and other fats through the bloodstream. They consist of a core of cholesterol and triglycerides surrounded by a shell of proteins, phospholipids, and cholesterol.
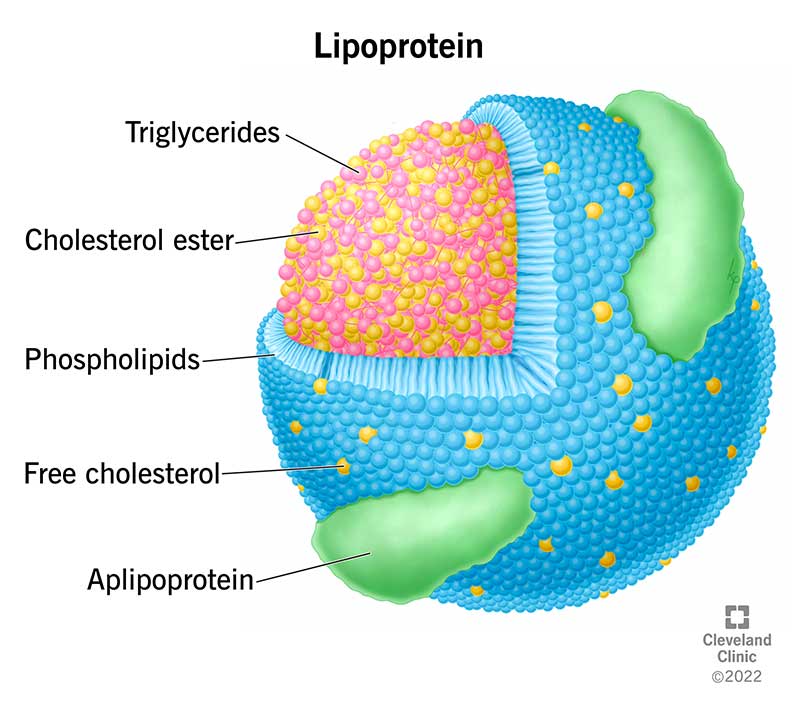
The main types, from lowest to highest density, are:
- Chylomicrons: Transport dietary fats from the intestines to other parts of the body.
- VLDL (very low-density lipoprotein): Carries triglycerides from the liver to tissues.
- IDL (intermediate-density lipoprotein): Formed as VLDL loses triglycerides.
- LDL (low-density lipoprotein): Often called "bad" cholesterol. It delivers cholesterol to tissues but can contribute to plaque buildup if there's too much.
- HDL (high-density lipoprotein): Often called "good" cholesterol. It helps remove excess cholesterol from tissues and arteries.
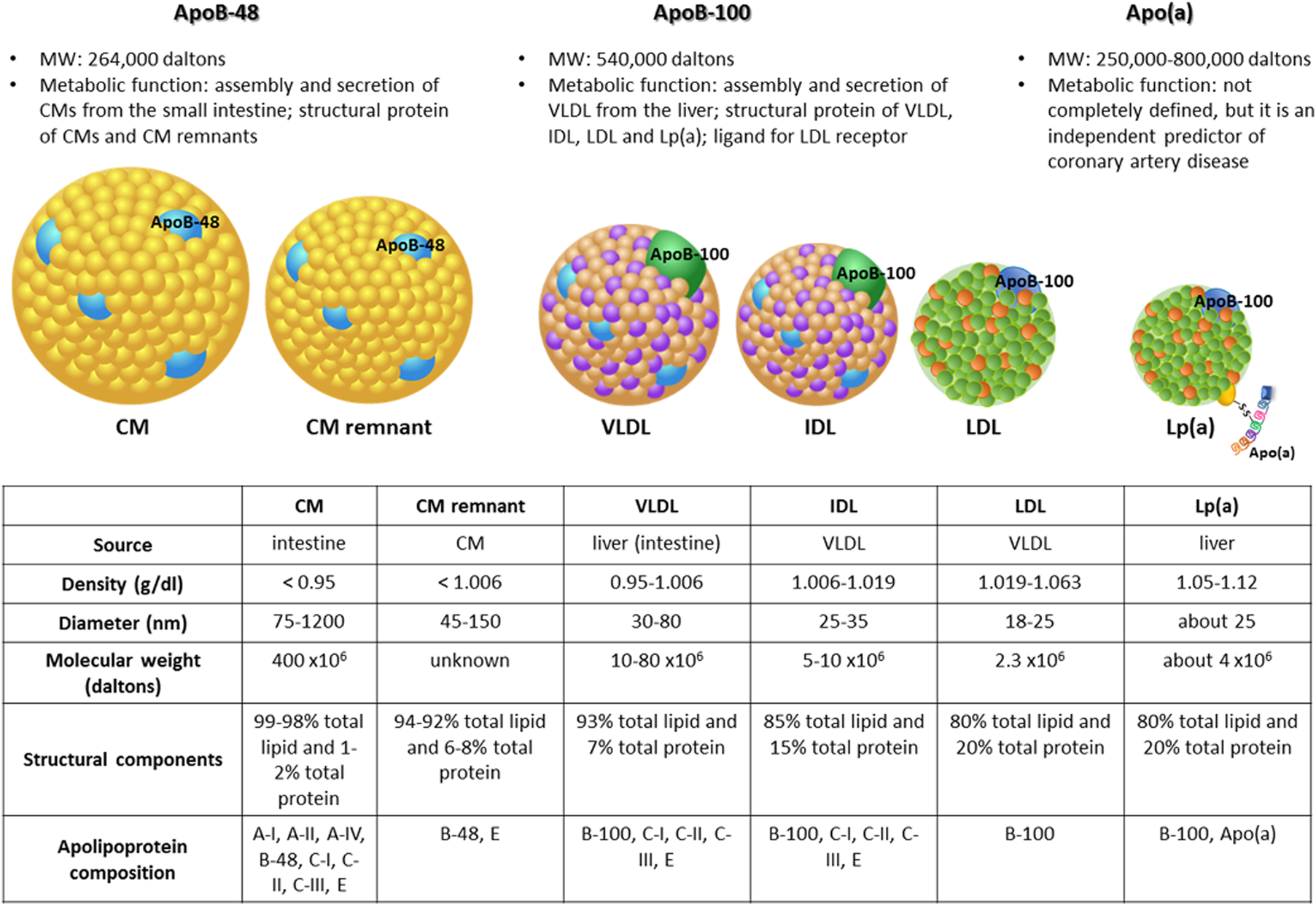
Apolipoprotein B (apoB)
- The primary protein component of all atherogenic lipoproteins.
- ApoB levels reflect the total number of potentially harmful particles, making it a better predictor of CVD risk than LDL cholesterol alone.
The HDL-LDL Balance
- While LDL can contribute to plaque formation, HDL helps remove excess cholesterol from the arteries.
- A healthy balance between these two is crucial for cardiovascular health.
Beyond LDL-C
- Traditional tests measure LDL-C (the amount of cholesterol within LDL particles).
- However, the number and size of LDL particles (measured by apoB or LDL-P tests) are often more informative about cardiovascular risk.
Understanding these components helps explain why simply lowering total cholesterol isn't always enough. The type, size, and number of lipoprotein particles play crucial roles in atherosclerosis risk.
Heart Attacks, Strokes, and Cardiovascular Disease
Now that we understand atherosclerosis, let's explore how it can lead to serious cardiovascular events:
- Heart Attacks (Myocardial Infarction):
- Occurs when a coronary artery (which supplies blood to the heart muscle) becomes blocked, usually due to a ruptured atherosclerotic plaque.
- The rupture triggers blood clot formation, cutting off blood supply to part of the heart muscle.
- Symptoms often include chest pain, shortness of breath, and pain radiating to the arm or jaw.
- Strokes:
- Ischemic stroke: Similar to a heart attack, but occurring in the brain. A blood clot blocks an artery supplying blood to part of the brain.
- Hemorrhagic stroke: When a weakened blood vessel in the brain ruptures. While not directly caused by atherosclerosis, hypertension (often associated with atherosclerosis) is a major risk factor.
- Symptoms can include sudden numbness, confusion, trouble speaking or understanding speech, vision problems, or severe headache.
- Peripheral Artery Disease (PAD):
- Atherosclerosis in arteries supplying the limbs, most commonly the legs.
- Can cause pain when walking (claudication) and, in severe cases, tissue death (gangrene).
- Aneurysms:
- Weakening of the artery wall, causing it to bulge outward.
- While not directly caused by atherosclerosis, they often occur in arteries damaged by the atherosclerotic process.
- If an aneurysm ruptures, it can cause life-threatening internal bleeding.
- Chronic Kidney Disease:
- Atherosclerosis in the renal arteries can reduce blood flow to the kidneys, impairing their function.
- Angina:
- Chest pain or discomfort caused by reduced blood flow to the heart due to narrowed coronary arteries.
- Often a warning sign of more serious heart problems.
Understanding these potential outcomes underscores the importance of preventing and managing atherosclerosis. Early detection and intervention can significantly reduce the risk of these life-threatening events.
Prevention Strategy
The general strategy to prevent atherosclerosis is to manage your blood pressure, control inflammation, and optimize your lipid profile. The goal is to get your apoB levels down to extremely low levels (30-40 mg/dL) and keep them there, while also managing other risk factors like blood pressure, inflammation, and blood sugar. It will almost certainly require pharmacological intervention, but lifestyle changes can also have a significant impact.
Here is the general approach to preventing atherosclerosis:
- Monitor Key Biomarkers:
- Regular check-ups and blood tests are crucial.
- Focus on apoB levels, aiming for 30-40 mg/dL
- Monitor blood pressure, lipid profiles, and other cardiovascular risk factors
- Medication:
- If prescribed, take medications to lower your apoB levels.
- Common medications include statins, PCSK9 inhibitors, and blood pressure medications.
- Always follow your healthcare provider's advice regarding medication.
- Diet:
- Focus on anti-inflammatory foods and those that help manage blood pressure and apoB levels.
- Adopt a Mediterranean-style diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit saturated fats, processed foods, and added sugars.
- Exercise:
- Engage in regular physical activity for cardiovascular fitness and metabolic health.
- Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Include both cardio and strength training in your routine.
- Lifestyle:
- Manage stress through techniques like meditation, yoga, or deep breathing exercises.
- Prioritize sleep, aiming for 7-9 hours of quality sleep per night.
- Quit smoking and limit alcohol consumption.
- Maintain a healthy weight.
- Regular Screenings:
- Schedule regular check-ins with your healthcare provider
- Undergo recommended screenings based on your age, gender, and risk factors
Monitoring
Blood Pressure
- Frequency: At least annually during regular check-ups; more frequently if you have hypertension (up to multiple times per week).
- Methods:
- Annual physical (note: single readings may not be the most reliable)
- Local pharmacy machines
- Home blood pressure monitor (recommended for those with concerns)
- Target: Below 120/80 mmHg, ideally closer to 115/75 mmHg
- Note: Generally, lower is better within a healthy range
Advanced Lipid Panels
Standard lipid profile testing has limited value compared to more advanced lipid testing methods. While you'll get a standard lipid panel at your annual physical, focus on advanced markers, particularly apolipoprotein B (apoB) levels and lipoprotein particle numbers, for a more accurate assessment of cardiovascular risk.
Key Measurements
- Standard Lipid Panel (annual physical)
- Advanced Lipoprotein Testing
- Lipoprotein particle numbers and sizes
- Apolipoprotein measurements
- Lipoprotein(a) [Lp(a)] (one-time test for genetic risk assessment)
Frequency
- Initially: My recommendation is to get these tests done at least once a year, ideally every 6 months if you're actively working on lowering your apoB levels.
- Ideally: Every 3-6 months to track progress, or more frequently if adjusting medications or lifestyle factors. Can settle back to annual testing once things stabilize if needed.
- Adjust based on risk factors and treatment plan with your healthcare provider.
- In general, I think you should be targeting neonatal levels of apoB (30-40 mg/dL) and keeping them there, which will likely require pharmacological intervention... don't be afraid to push for more aggressive treatment than the reference ranges suggest.
Sample Advanced Lipid Panel Results
| Test Name | Units | Result | Risk Category | Optimal | Moderate | High |
|---|---|---|---|---|---|---|
| Lipid Panel | ||||||
| CHOLESTEROL, TOTAL | mg/dL | 274 | High | <200 | N/A | >=200 |
| HDL CHOLESTEROL | mg/dL | 91 | Optimal | >=50 | N/A | <50 |
| TRIGLYCERIDES | mg/dL | 102 | Optimal | <150 | 150-199 | >=200 |
| LDL-CHOLESTEROL | mg/dL | 161 | High | <100 | 100-129 | >129 |
| CHOL/HDLC RATIO | calc | 3.0 | Optimal | <=3.5 | 3.6-5.0 | >5.0 |
| NON-HDL CHOLESTEROL | mg/dL (calc) | 183 | Moderate | <130 | 130-189 | >=190 |
| Lipoprotein Subfractions | ||||||
| LDL PARTICLE NUMBER | nmol/L | 1240 | Optimal | <1260 | 1260-1538 | >1538 |
| LDL SMALL | nmol/L | 142 | Optimal | <162 | 162-217 | >217 |
| LDL MEDIUM | nmol/L | 183 | Optimal | <201 | 201-271 | >271 |
| HDL LARGE | nmol/L | 6927 | High | >9386 | 9386-6996 | <6996 |
| Apolipoproteins | ||||||
| APOLIPOPROTEIN B | mg/dL | 118 | Moderate | <80 | 80-119 | >=120 |
| LIPOPROTEIN (a) | nmol/L | 253 | High | <75 | 75-125 | >125 |
Note: All tests are from Lab: EZ according to the image.
Additional Considerations
-
ApoB and LDL-P: These are more predictive of cardiovascular risk than standard lipid panels. Prioritize these results when available.
-
Lp(a): Elevated levels indicate higher genetic risk for atherosclerosis. If elevated, manage other lipid markers (especially ApoB) more aggressively.
-
Lipoprotein Particle Analysis: Provides a comprehensive view of lipid-related risks, including particle numbers and sizes. This can be done through various technologies such as nuclear magnetic resonance (NMR) spectroscopy or ion mobility analysis.
-
Insulin Resistance: Some advanced lipid tests include an insulin resistance score. This is associated with insulin resistance and diabetes risk. Target score is typically ≤ 45, but may vary by test method.
Action Steps
- Request advanced lipoprotein testing, including particle numbers and apolipoprotein measurements, from your healthcare provider.
- If unavailable through your primary care physician, consider paying out-of-pocket for these advanced tests.
- Use results to guide lifestyle interventions and, if necessary, medication adjustments.
- Retest regularly, especially when making significant changes to diet, exercise, or medication regimen.
Interpreting Results
- Focus primarily on LDL-P and ApoB levels. Lower levels indicate lower cardiovascular risk.
- While other markers (e.g., Small LDL-P, LDL Size) provide additional information, their importance is secondary to total LDL-P and ApoB.
- Consider all markers in context with each other and your overall health profile.
Remember to work closely with your healthcare provider to interpret results and develop a personalized treatment plan based on your overall health profile and risk factors. The specific advanced testing method used may vary, but the key is to obtain detailed information about lipoprotein particles and apolipoproteins beyond what's available in a standard lipid panel.
Visual Scans
Visual scans provide direct imaging of coronary arteries, offering valuable insights into the presence and extent of atherosclerosis. The two primary options are Coronary Artery Calcium (CAC) scans and Coronary CT Angiography (CCTA).
When to Start and How Often
- Initial Screening: Consider a CAC scan around age 40-45 for men and 50-55 for women, earlier if multiple risk factors are present.
- Follow-up: If initial CAC score is zero, repeat every 5 years. For non-zero scores, frequency depends on the score and risk factors.
- CCTA: Typically not used for initial screening. Consider if CAC score is high or if symptoms develop.
Coronary Artery Calcium (CAC) Scan
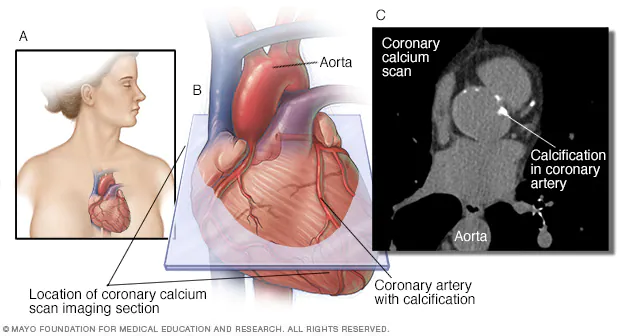
- How it works: Non-invasive CT scan without contrast; detects and quantifies calcified plaque in coronary arteries
- Result: Provides a "calcium score" indicating atherosclerosis extent
- Best for: Screening and risk stratification in asymptomatic, intermediate-risk patients
- Clinical utility:
- Excellent for detecting presence of atherosclerosis
- Strong predictor of future cardiovascular events
- Guides preventive therapies
- Practical aspects:
- Quick procedure (10 minutes)
- Low radiation exposure
- Cost: $100-$400, often not covered by insurance for screening
- Widely available in most areas
- Limitations:
- Cannot detect non-calcified plaque
- No information on arterial stenosis
Coronary CT Angiography (CCTA)
- How it works: CT scan with intravenous contrast; provides detailed 3D images of coronary arteries
- Result: Visualizes both calcified and non-calcified plaque; assesses degree of arterial stenosis
- Best for: Detailed evaluation of symptomatic patients or those with high CAC scores
- Clinical utility:
- Detects presence, composition, and extent of plaque
- Evaluates suspected coronary artery disease
- Guides treatment decisions in known coronary artery disease
- Practical aspects:
- Higher radiation exposure than CAC
- Requires IV contrast (potential for allergic reactions)
- Cost: $500-$1,500, often covered for symptomatic patients
- Less widely available, typically in larger medical centers
- Limitations:
- Higher radiation and cost compared to CAC
- May lead to incidental findings requiring further workup
Strategy for Use
- Start with CAC scan for initial screening based on age and risk factors
- If CAC score is zero, consider repeating in 5 years
- For non-zero CAC scores, follow up more frequently based on the score and risk factors:
- Low score (1-100): Every 3-5 years
- Moderate score (101-400): Every 2-3 years
- High score (>400): Annually, and consider CCTA
- Consider CCTA if:
- CAC score is high
- Symptoms develop
- Detailed plaque characterization is needed
- Combine with advanced lipid testing for comprehensive risk assessment
- Adjust strategy based on changes in risk factors, symptoms, or test results
- Consult your healthcare provider to determine the most appropriate testing schedule based on your individual risk profile and test results
DEXA Scan
DEXA (Dual-Energy X-ray Absorptiometry) scans provide detailed body composition analysis, offering insights into fat distribution and lean mass that are relevant to cardiovascular and overall health.
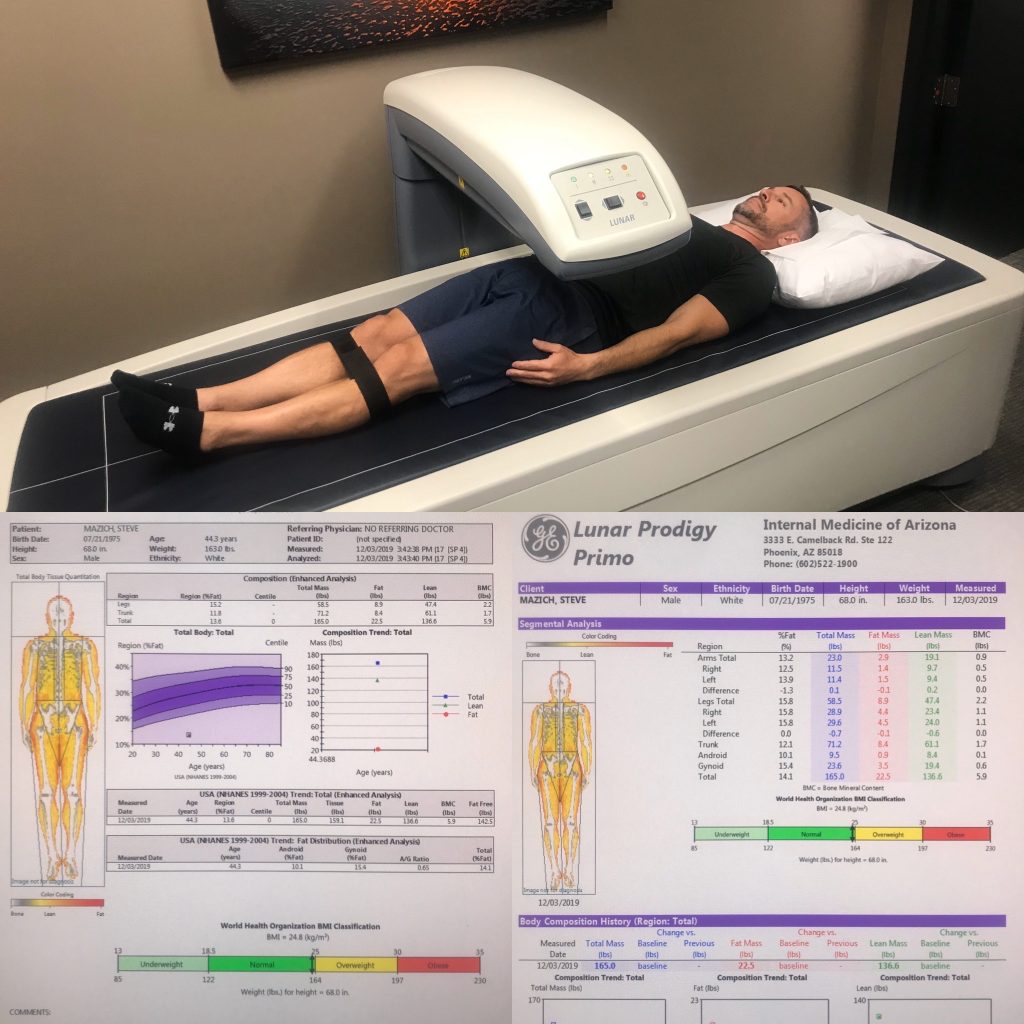
-
Body Fat Percentage:
- Men: 10-20% (athlete), 14-24% (fitness), 21-31% (acceptable), >32% (obese)
- Women: 18-28% (athlete), 21-31% (fitness), 25-35% (acceptable), >38% (obese)
-
Android/Gynoid Ratio (A/G Ratio):
- Men: < 1.0 is ideal
- Women: < 0.8 is ideal
- Higher ratios indicate more abdominal (android) fat, which is associated with increased cardiovascular risk
-
Visceral Adipose Tissue (VAT):
- < 100 cm² is considered low risk
- 100-160 cm² is moderate risk
- > 160 cm² is high risk
-
Lean Mass Index (LMI):
- Men: 18-22 kg/m² is average
- Women: 15-19 kg/m² is average
- Higher values indicate more muscle mass, which is generally beneficial for metabolic health
-
Bone Mineral Density (BMD):
- T-score > -1.0 is normal
- T-score between -1.0 and -2.5 indicates osteopenia
- T-score < -2.5 indicates osteoporosis
Key Measurements Indicative of Health:
-
Body Fat Percentage: Lower values within the healthy range are associated with better cardiovascular health.
-
A/G Ratio: Lower ratios indicate a more favorable fat distribution pattern, with less abdominal fat.
-
Visceral Adipose Tissue (VAT): Lower VAT levels are strongly associated with reduced cardiovascular and metabolic risk.
-
Lean Mass Index (LMI): Higher LMI values, indicating more muscle mass, are associated with better metabolic health and longevity.
-
VAT/Total Fat Ratio: A lower proportion of visceral fat to total body fat is preferable for metabolic health.
-
Bone Mineral Density: Higher BMD values indicate stronger bones and lower risk of osteoporosis.
- Frequency: Annually or as needed to track body composition changes.
- Tests: Body fat percentage, lean mass distribution, visceral fat levels, bone mineral density.
- Target: Healthy body fat percentage, low visceral fat levels, balanced lean mass distribution, and normal bone density.
Interpreting Results for Cardiovascular Health:
- Focus on reducing visceral fat (VAT) if levels are high, as this fat type is most strongly linked to cardiovascular risk.
- Aim to increase or maintain lean mass, which is associated with better insulin sensitivity and metabolic health.
- Monitor changes in A/G ratio over time; decreases in this ratio often correlate with improvements in metabolic health.
- Use DEXA results in conjunction with blood tests (lipids, glucose) for a comprehensive cardiovascular risk assessment.
Remember that DEXA scans provide valuable data, but should be interpreted in the context of overall health, lifestyle, and other risk factors. Consult with a healthcare professional to develop a personalized plan based on your DEXA results.
Cardiovascular Health
I would strongly recommend using something like an Apple Watch to get a convenient way to monitor various aspects of your cardiovascular health. That will make it really easy to track things like resting heart rate, heart rate variability, step counts, etc. You'll also get an ongoing estimate of VO2 max based on workout performance. In addition to the fitness / health tracker, I would recommend getting an annual VO2 max test.
Here are key metrics you can track:
Resting Heart Rate (RHR)
- What it is: The number of times your heart beats per minute while at rest.
- How to measure: Your Apple Watch automatically measures this throughout the day and night. Otherwise, you can manually check your pulse when you wake up.
- Where to find it: Health app > Browse > Heart > Resting Heart Rate
- Why it's important: RHR is an indicator of cardiovascular fitness. A lower RHR generally indicates better fitness.
- Interpretation:
- Excellent: 60-70 bpm
- Good: 70-80 bpm
- Average: 80-90 bpm
- Poor: >90 bpm
- Tips: Check your trends over time. A gradual decrease often indicates improving fitness.
Heart Rate Variability (HRV)
- What it is: The variation in time between heartbeats.
- How to measure: Your Apple Watch measures this automatically, typically during sleep.
- Where to find it: Health app > Browse > Heart > Heart Rate Variability
- Why it's important: HRV reflects your nervous system balance and recovery state. Higher HRV generally indicates better stress resilience.
- Interpretation: HRV is highly individual. Focus on your personal trends over time rather than absolute numbers.
- Tips: Consistently higher HRV often correlates with better fitness and lower stress.
Activity and Exercise Data
- What to track: Daily steps, stand hours, exercise minutes, and active calories burned.
- How to measure: Wear your Apple Watch throughout the day.
- Where to find it: Activity app or Health app > Activity
- Why it's important: Regular physical activity is crucial for cardiovascular health.
- Interpretation:
- Move Goal: Set personally challenging active calorie target
- Exercise Goal: Aim for at least 30 minutes daily
- Stand Goal: Try to stand for at least 1 minute in 12 different hours
- Tips: Use the "Trends" feature in the Activity app to see how your metrics change over time.
Cardio Fitness (VO2 Max Estimate)
- What it is: An estimate of the maximum rate of oxygen consumption during exercise.
- How to measure: Automatically estimated by Apple Watch during outdoor walks, runs, or hikes of at least 20 minutes.
- Where to find it: Health app > Browse > Heart > Cardio Fitness
- Why it's important: It's a good indicator of overall cardiovascular fitness.
- Interpretation: Apple provides a classification based on your age and gender:
- Low
- Below Average
- Above Average
- High
- Tips: To improve accuracy, ensure your physical details (height, weight, etc.) are up to date in the Health app.
| Metric | Poor | Average | Good | Excellent |
|---|---|---|---|---|
| Resting Heart Rate (bpm) | >90 | 80-90 | 70-80 | 60-70 |
| HRV (ms) | Focus on personal trends rather than absolute values | |||
| Daily Move Goal | Not meeting | Meeting 50-75% | Meeting 75-100% | Exceeding |
| Daily Exercise Minutes | <15 | 15-29 | 30-60 | >60 |
| Cardio Fitness | Low | Below Average | Above Average | High |
How to Use These Metrics:
-
Check Regularly: Review your metrics weekly to understand your baseline and track changes.
-
Look for Trends: Focus on long-term trends rather than daily fluctuations.
-
Set Realistic Goals: Use the Apple Watch's suggestion feature to set achievable activity goals.
-
Use Guided Features: Try the Fitness+ workouts or Mindfulness app to improve your metrics.
-
Enable Notifications: Set up heart rate notifications to alert you of unusual patterns.
-
Share with Your Doctor: Apple Health allows you to generate reports to share with healthcare providers.
Remember, while Apple Watch provides valuable insights, it's not a medical device. Use these metrics as motivation for a heart-healthy lifestyle, including regular exercise, a balanced diet, stress management, and adequate sleep. Always consult with a healthcare professional for medical advice and before starting any new fitness regimen.
VO2 Max Testing
VO2 max is the maximum rate of oxygen consumption measured during incremental exercise. It's considered the gold standard for assessing cardiovascular fitness and endurance capacity.
Test Procedure
-
Preparation:
- Avoid heavy exercise 24 hours before the test
- Don't eat a large meal 2-3 hours before testing
- Wear comfortable exercise clothing and appropriate footwear
-
Equipment:
- Treadmill or stationary bike
- Breathing mask or mouthpiece
- Heart rate monitor
- Gas analyzer
-
Protocol:
- Begin with a warm-up period
- Exercise intensity increases gradually
- Continue until exhaustion or predetermined criteria are met
- Typically lasts 8-12 minutes
Interpreting VO2 Max Test Results
VO2 max is usually expressed in milliliters of oxygen per kilogram of body weight per minute (ml/kg/min).
Reference Ranges (ml/kg/min)
| Age | Poor | Fair | Good | Excellent | Superior |
|---|---|---|---|---|---|
| 20-29 | <33 | 33-36 | 37-41 | 42-46 | >46 |
| 30-39 | <31 | 31-34 | 35-39 | 40-44 | >44 |
| 40-49 | <28 | 28-31 | 32-36 | 37-41 | >41 |
| 50-59 | <25 | 25-28 | 29-33 | 34-38 | >38 |
| 60+ | <23 | 23-26 | 27-31 | 32-36 | >36 |
Note: These ranges are for men. Women's values are typically about 10% lower.
Factors Affecting VO2 Max
- Age
- Gender
- Genetics
- Training status
- Body composition
- Altitude
Improving VO2 Max
- High-Intensity Interval Training (HIIT)
- Endurance training
- Altitude training
- Proper nutrition and hydration
- Adequate recovery and sleep
Frequency of Testing
- Initially: Establish a baseline
- Progress tracking: Every 3-6 months
- After significant changes in training regimen
Remember, while VO2 max is an excellent indicator of cardiovascular fitness, it's just one aspect of overall health. Combine this information with other metrics and consult with healthcare professionals for a comprehensive fitness assessment.
Tracking Details
In general, whether you use a Habit Tracking app like Streaks, Apple Watch / Health, and/or just a spreadsheet, I would strongly recommend reviewing everything on a nightly, weekly, monthly, quarterly, and yearly basis. Look at the numbers, the stats, and some charts / visualizations.
- Use a habit tracking app like Streaks
- Get an Apple Watch, Oura Ring, etc. for passive monitoring and data collection
- Use a spreadsheet to keep track of the detailed data
- Analyze trends, statistics (i.e. outliers, standard deviation, etc.), and visualizations to gain insights into your overall health trajectory
- Review key data on a nightly, weekly, monthly, quarterly, and yearly basis
- Nightly: Did I eat red meat, did I drink alcohol, etc...
- Weekly: How many hours of zone 2 cardio did I do? How was my sleep, etc.
- Monthly: Similar to weekly
- etc...
Drugs
- Statins: These are the first-line treatment for lowering cholesterol. Examples include atorvastatin (Lipitor) and rosuvastatin (Crestor). They work by inhibiting an enzyme involved in cholesterol production in your liver. Potential concerns: While generally safe and effective, some people experience side effects like muscle pain. Regular liver function monitoring is necessary. The benefits often outweigh the risks for those at high risk of CVD.
- PCSK9 inhibitors: Consider these if statins are ineffective or poorly tolerated. Examples include evolocumab (Repatha) and alirocumab (Praluent). They work by allowing your liver to remove more LDL from your bloodstream.
- Blood Pressure Medications: Various types exist, including ACE inhibitors, ARBs, and calcium channel blockers. Work with your doctor to find the right fit while avoiding medications that may raise blood pressure unnecessarily if needed
- Hypertension: Avoid medications that raise blood pressure if possible (e.g., certain decongestants, NSAIDs, stimulants like Adderall, ED medications like Viagra). If you need these medications, work closely with your doctor to monitor and manage blood pressure.
Diet / Nutrition
- Mediterranean-style diet: Focus on high-protein foods, healthy fats, and plenty of vegetables. Eat fiber-rich foods like legumes and whole grains; fiber helps lower cholesterol by binding to it in the digestive system.
- Manage fats: Reduce saturated fat intake (cheese, fatty red meats, etc.). Aim for lean cuts of meat and limit red meat to 1-2 meals per week maximum.
- Carbohydrate control: Follow a low-sugar diet to prevent inflammation, insulin resistance, and increased triglyceride levels. Limit simple carbs, especially processed ones, as they rapidly convert to glucose, spiking blood sugar and insulin levels.
- Meal timing: Time carb intake for post-workout or later in the day when insulin sensitivity may be higher. Consider time-restricted eating, such as skipping breakfast and starting with black coffee and water. However, if you struggle to get enough calories or tend to eat unhealthily when skipping meals, maintain a regular eating schedule.
- Post-meal activity: Walk after high-carb meals to help mitigate blood sugar spikes.
- Sodium intake: Moderate sodium intake to less than 2300mg per day, or even lower if you're salt-sensitive. If you sweat a lot, you may need more salt than the average person.
- Hydration: Drink primarily water. Avoid drinking your calories through sugary beverages like sodas or fancy coffee drinks.
- Supplementation: Consider fish oil and vitamin D supplements. Take magnesium/zinc at night to help with deeper sleep. If you lift weights, consider adding whey protein isolate and creatine to your supplement regimen.
- Coffee consumption: Enjoy coffee for its health benefits, but be mindful of excessive caffeine intake, which can temporarily raise blood pressure.
- Alcohol moderation: Limit alcohol consumption to 1-2 drinks maximum when you do drink. Have them earlier in the day rather than right before bed, and limit drinking to once a week or 1-2 days per month. Choose quality over quantity (e.g., a great scotch or nice wine over a six-pack of beer).
- Dietary cholesterol: Don't worry too much about dietary cholesterol (e.g., from eggs) as it has minimal impact on blood cholesterol for most people. Your body synthesizes most of the cholesterol it needs.
Exercise / Activity
Regular physical activity is like a magic pill for heart health. It strengthens your heart, improves circulation, and helps manage risk factors like high blood pressure and unhealthy cholesterol levels. Here's how to get moving:
- "Zone 2" Cardio: This is your cardiovascular sweet spot. Aim for 3+ hours weekly at 60-70% of your maximum heart rate. It's an intensity where you can still hold a conversation but are definitely working. I like the stairmaster or elliptical machines the best, some people swear by exercise bikes, etc. You can probably just use an Apple Watch to monitor heart rate, or can get more accurate reading with chest band, or even use a lactate meter to get really dialed in. I usually do mine while watching sports, movie / TV show, or while listening to a good podcast. Ideally you'll get 3+ hours every week of this type of cardio... but even just doing 30 minutes has a massive positive impact compared to doing nothing.
- HIIT (High-Intensity Interval Training): Incorporate short bursts of intense activity for improved VO2 max. The Norwegian 4x4 protocol (4 sets of 4-minute high-intensity intervals with 3 minutes of active recovery) is an effective option.
- Strength Training: Don't neglect your muscles. Resistance training improves metabolic health and body composition, indirectly benefiting your heart.
- Daily Movement: Increase general physical activity through daily habits. Take walks after dinner, go hiking, engage in active hobbies, etc. Consider a treadmill desk or under-desk bike for extra movement during the day. Park farther away, take the stairs at work, etc.
- Sweat it Out: Consider regular sauna sessions for potential cardiovascular benefits. Aim for 2-3 sessions per week, 15-20 minutes each time, if tolerated.
Remember, the best exercise is the one you'll actually do consistently. Find activities you enjoy and make them a regular part of your routine.
Sleep
Quality sleep is crucial for cardiovascular health, metabolic function, and overall well-being. During sleep, your body repairs tissues, regulates hormones, and manages stress. Aim for 7-9 hours of quality sleep per night and maintain consistent sleep patterns.Poor sleep is associated with increased inflammation, insulin resistance, and higher blood pressure - all risk factors for atherosclerosis.
Lifestyle / Stress
Your daily habits and stress levels have a significant impact on heart health:
- Kick the Habit: If you smoke, quitting is one of the best things you can do for your heart. Seek support if needed.
- Stress Less: Implement stress management techniques like meditation, deep breathing exercises, or engaging in hobbies you enjoy.
- Clean Air: Be mindful of air quality. Consider air purifiers for your home if you live in a high-pollution area.
- Social Connections: Maintain strong social bonds. Positive relationships can help manage stress and promote overall well-being.
Key Recommendations
- Lower apoB levels to 30-40 mg/dL through diet, exercise, and medication if needed.
- Prioritize regular cardio exercise, especially "Zone 2" training.
- Adopt an anti-inflammatory diet focused on whole foods.
- Ensure consistent, quality sleep of 7+ hours nightly.
- Regularly monitor key biomarkers and adjust your strategy as needed.
Actions: Your Next Steps
- Initial Evaluation: Schedule appointment with primary care physician, get a comprehensive lipid panel done that includes apoB measurement and a one time test for Lp(a) to understand genetic risks. Discuss your cardiovascular risk factors and potential need for futher tests (e.g. CAC scan) and/or medication (e.g. low grade statin)
- Improve Your Diet: Plan your meals for the next week, focusing on a Mediterranean style diet
- Start Exercising: Start with modest goal such as a 30 minute brisk walk 5 days a week. Get into the routine of exercising
- Start Tracking: Get an Apple Watch (or equivalent) to monitor heart rate and activity levels, measure your blood pressure regularly, use a notebook/app/spreadsheet to keep track of your exercise and other important habits and activities
- Monitor: Make it a habit to review your various data regularly to keep yourself accountable and make adjustments as needed
Conclusion
Atherosclerosis is a serious but largely preventable condition. By understanding the process, monitoring key health indicators, and adopting heart-healthy habits, you can significantly reduce your risk of cardiovascular disease. Remember, it's never too early or too late to start taking care of your heart. Preventing atherosclerosis is a lifelong journey. Start with small, sustainable changes and gradually build on your successes. Consult with your healthcare provider to create a personalized plan that works best for you. Your future self will thank you for the steps you take today!
Misc Questions
Q: Why do traditional bloodwork tests measure LDL and not apoB?
A: Traditional lipid panels measure LDL-C (LDL cholesterol), which represents the amount of cholesterol within LDL particles. However, apoB provides a more accurate measure of cardiovascular risk as it represents the actual number of atherogenic particles. Here's why apoB is considered superior:
- Comprehensive measurement: ApoB is found on all atherogenic lipoproteins (LDL, VLDL, and Lp(a)), providing a complete picture of potentially harmful particles.
- Direct particle count: Each atherogenic particle contains one apoB molecule, making it a direct measure of the number of particles, not just their cholesterol content.
- Reflects particle size: ApoB better accounts for small, dense LDL particles, which are particularly atherogenic but may be underrepresented by LDL-C measurements.
- Stronger predictor: Multiple studies and meta-analyses have shown apoB to be superior to LDL in predicting cardiovascular risk, even when LDL levels are normal or low.
- Stable measurement: ApoB levels are less affected by fasting status, providing more consistent results.
- Valuable in treated patients: ApoB remains predictive in patients treated with statins, where LDL may lose some predictive power.
Despite these advantages, the medical community has been slow to adopt apoB as the primary measure due to:
- Established guidelines and treatment targets based on LDL-C
- Wider availability and lower cost of LDL-C testing
- Familiarity among healthcare providers with LDL-C interpretation
However, many experts now recommend measuring apoB, especially for patients with metabolic syndrome, diabetes, or those at intermediate cardiovascular risk. Always discuss with your healthcare provider about including apoB in your lipid panel for a more comprehensive assessment of your cardiovascular health.
Q: What about the carnivore diet? Some say saturated fat isn't as bad as we thought.
A: While some studies suggest saturated fat may not be as harmful as previously believed, the overall body of evidence still supports limiting saturated fat intake for heart health. The carnivore diet is highly controversial and lacks long-term studies on its effects. Most health organizations recommend a balanced diet rich in fruits, vegetables, and whole grains for optimal health. In my personal opinion, you should limit red meat to 1-2 meals per week and try to stick with the leaner cuts. That said, getting advanced apolipoprotein profiling labs done (e.g. Nuclear Magnetic Resonane Lipoprofile, Ion Mobility Analysis, etc.) might give you more insight into the range of particle sizes / concentrations which could inform your risk / reward better.
Q: Are there concerns about taking statins?
A: Statins are generally safe and effective, but like all medications, they can have side effects. The most common is muscle pain or weakness. Rarely, they can cause liver problems or increase diabetes risk. However, for most people at high risk of CVD, the benefits of statins outweigh the potential risks. Always discuss concerns with your healthcare provider.
Q: How does exercise specifically help prevent atherosclerosis?
A: Regular exercise offers multiple benefits for preventing atherosclerosis:
- Improves lipid profile: Increases HDL cholesterol and may reduce LDL and triglycerides.
- Lowers blood pressure: Reduces strain on artery walls.
- Enhances endothelial function: Improves the health and function of the arterial lining.
- Reduces inflammation: Regular exercise has anti-inflammatory effects.
- Improves insulin sensitivity: Helps maintain healthy blood sugar levels.
- Stress reduction: Acts as a natural stress reliever.
- Weight management: Helps maintain a healthy body weight, reducing metabolic risk factors.
Both aerobic exercise and strength training contribute to these benefits, emphasizing the importance of a well-rounded fitness routine.
Q: How does sleep affect atherosclerosis risk?
A: Sleep plays a crucial role in cardiovascular health:
- Blood pressure regulation: During normal sleep, blood pressure drops. Chronic sleep deprivation can lead to hypertension.
- Inflammation: Poor sleep quality or duration increases inflammatory markers associated with atherosclerosis.
- Metabolic effects: Sleep deprivation can lead to insulin resistance and weight gain.
- Stress hormones: Lack of sleep increases cortisol levels, potentially damaging blood vessels over time.
- Repair processes: Sleep is when the body performs many repair functions, including in the cardiovascular system.
Aim for 7-9 hours of quality sleep per night. If you have sleep disorders like sleep apnea, seek treatment, as these conditions significantly increase cardiovascular risk.
